LET'S talk ABOUT TONGUE TIES IN ADULTS
WHAT ARE THEY AND WHY SHOULD YOU CARE?
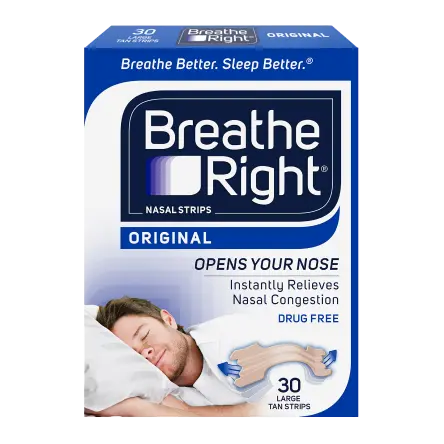
While many times a lingual restriction is identified as an infant or child, adults can still have a tongue tie. In adult patients, we may see signs and symptoms like sleep disordered breathing, dental crowding, teeth grinding, and TMJ issues.
If we suspect a tongue tie, we will recommend an airway workup to evaluate how a tongue tie may be impacting the patient in the context of tongue tone, tongue space and symptoms and sleep.
In adults the procedure to address a tongue tie is called a functional frenuloplasty. This procedure removes restricted oral tissue includes sutures for optimal healing.
By working closely with a myofunctional therapist both before and after a procedure, we can ensure our adult patients’ recovery is as smooth and successful as possible. Myofunctional therapy will help patients improve oral muscle function and flexibility, as well as support lifestyle changes to maintain good oral health.
Most importantly, regardless of what stage or age we meet, there are options for all ages to help patients breathe, sleep, eat, communicate, and thrive.
How do we treat children & adults with tethered oral tissues?
Frenuloplasty
A frenuloplasty is a procedure performed to remove large, tight, or poorly positioned band(s) of tissue inside the mouth, connected to the lip, cheeks or floor of the mouth (frenum). Once the tissue has been removed, the area will be sutured. These restrictions are commonly referred to as being “tongue-tied” or “ankyloglossia”, but can be found in cheeks, lips or tongue, and we refer to them as “tethered oral tissues” or TOTs.
This procedure may be performed to improve eating, swallowing, mouth breathing, or myofunctional habits.
Frenuloplasty is a routine procedure and is often performed with just local anesthesia in adults and children.

MYOFUNCTIONAL THERAPY
Myofunctional therapy is an important aspect of both pre- and post-operative care for a functional frenuloplasty procedure. Before the surgery, it helps to prepare the oral and facial muscles for the changes that will occur, reducing the risk of complications and promoting faster recovery. After the procedure, myofunctional therapy helps to retrain the muscles to function in their new, correct position, reducing the risk of relapse and promoting long-term success.
It can help alleviate any discomfort or pain that may occur after the surgery and improve the overall function and appearance of the oral and facial structures. Myofunctional therapy is a critical component of a comprehensive treatment plan for functional frenuloplasty, helping to ensure optimal results and improved oral health.
What We
Evaluate:
- Space for teeth & tongue
- Breathing & facial muscle habits
- Sleep
- “Tongue tie”
How We
Evaluate:
- Clinical exam, CBCT 3D imagining
- Myofunctional screening
- Sleep screening
- Tongue range of motion mesurements
With all of this information, we can help determine what treatments may be needed and in what order. This saves valuable time and resources, and helps prevent or treat breathing or sleep disorders while also creating healthy and beautiful smiles.
How we might treat
01
Tongue Space
Myofunctional Orthodontics
02
Tongue Tone
Myofunctional Therapy
03
Tongue Tie
Functional Frenuloplasty
02
Involve other Specialists as needed
For example: Ear, nose and throat doctors may be consulted regarding tonsils and adenoids and allergies.

Our Goals At The MyoGrow Airway Center:
Tongue up
Lips closed
Healthy swallow pattern
Nasal breathing
Forward facial growth
MyoGrow Frequently Asked Questions
At the MyoGrow Airway Center we envision a world where we can help infants, children and adults breathe, sleep, eat, communicate, grow, and thrive through myofunctional orthodontics, releasing tethered oral tissues, and collaborating with airway health colleagues.
What is “Myogrow”?
Our pediatric airway program goes by the name of Myogrow. It encompasses the assessment and management of tethered oral tissues (TOTs), development of the head and neck, breathing patterns, and myofunctional habits, i.e., the manner in which we use our muscles and body to breathe, sleep, eat, and speak. Here’s a video that explains more: https://www.youtube.com/watch?v=LTnSo6YDEkQ&t=9s
Why haven’t other providers talked to me about myofunctional issues?
These concepts are relatively new. Some providers may not be familiar with them yet. We strive to remain current with the latest research and work in collaboration with other healthcare professionals who do the same. Our approach involves a comprehensive evaluation of craniofacial growth patterns, as well as an assessment of sleeping, breathing, eating, and swallowing habits. This integration of factors is distinctive and requires expertise across various specialties.
What if I don’t have any concerns with my child’s sleeping or dental health.
These concepts are relatively new. Some providers may not be familiar with them yet. We strive to remain current with the latest research and work in collaboration with other healthcare professionals who do the same. Our approach involves a comprehensive evaluation of craniofacial growth patterns, as well as an assessment of sleeping, breathing, eating, and swallowing habits. This integration of factors is distinctive and requires expertise across various specialties.
What if I don’t have any concerns with my child’s sleeping or dental health?
If you do not have any immediate concerns regarding your child’s sleeping or dental health, we still suggest that you have them screened at least once between the ages of 4-11. Occasionally, early intervention is necessary to address specific concerns that the screening reveals and/or to ensure that growth is progressing in the appropriate direction. Remember, even if your child does not require immediate treatment, preventive measures can be taken to establish healthy habits that promote proper growth and development.
What can I expect during the initial “records” visit?
During the initial “records” visit, we will gather various forms of information to aid in our evaluation and treatment planning. This includes taking photos, measurements, medical history, and conducting a CT scan of the airway, as well as obtaining a digital scan of the teeth. After compiling and analyzing this data, we will share our findings and treatment recommendations with you (the parents) via a virtual Zoom meeting.